A tick bite is never something to brush off, forget about, or deal with later. Many ticks carry microbes that can cause a variety of diseases.
If diseases caused by tick bites are left untreated, they can lead to serious health problems that could potentially affect your muscles, joints, brain, heart, vision, and nervous system. Many tick-borne illnesses can have serious consequences that alter your lifestyle and activities by limiting your mobility, cognition, and overall quality of life. Knowing how to identify a tick bite and recognizing the general symptoms of tick-borne diseases can alert you to possible health risks sooner, so you can consult with your healthcare provider about appropriate next steps as soon as possible.
Identifying Ticks
What a tick looks like
The first step in identifying tick bites is to know what ticks look like. Belonging to the arachnid class (scorpions, spiders, mites), ticks begin their life as an egg, then hatch as a larva, which grows into a nymph and finally an adult tick. Ticks will look different at each stage of their life cycle.
Dozens of tick species exist. The different species of ticks may have alternating colorations or patterns, but they all have similar appearances, generally. Ticks are usually tiny, with some the size of a peppercorn. They typically have eight legs, a small head, and a body that is divided into one or two segments, depending on the type of tick. Most are brown, tan, or black, but numerous variations exist.
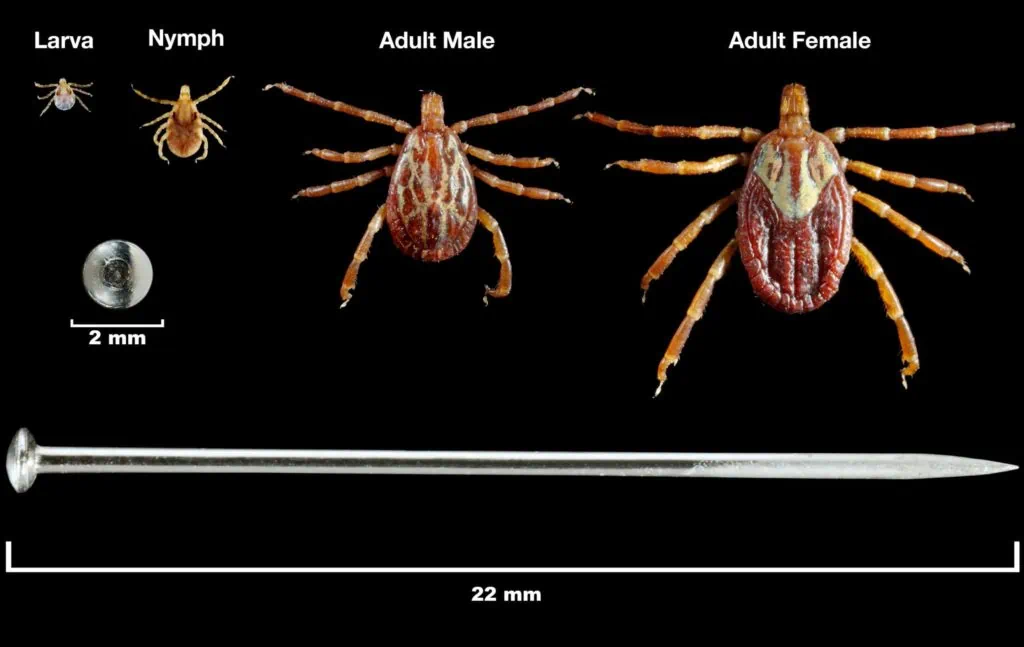
Ticks generally have four stages of life: egg, larvae, nymph and adult. Ticks advance through each of these stages by molting, a process during which they shed their outer skin.
Types of ticks
Ticks are usually categorized into two broad categories: hard ticks (Ixodidae) and soft ticks (Argasidae). Here is a brief rundown of a few different types of ticks found in the US.
- Blacklegged tick (also known as a deer tick)
- Western blacklegged tick
- Lone star tick
- American dog tick
- Brown dog tick
- Gulf coast tick
- Rocky Mountain wood tick
That said, ticks are not a problem exclusive to the United States by any measure. Ticks exist all over the world, including Europe and Canada.
Want more information about identifying the different types of ticks? Read IGeneX’s in-depth article on tick identification here.
The tick life cycle
Ticks have four stages of life: egg, larvae, nymph and adult. Ticks advance through each of these stages by molting, a process during which they shed their outer skin. When feeding occurs in the tick lifecycle heavily depends on the precise species of tick.
What does a tick bite look like?
If you’re worried you may have been exposed to a tick-borne illness, it’s obvious to wonder what a tick bite looks like. Unless a rash appears, a tick bite is likely to look much like any other bug bite.
So how do you know if you have a tick bite? The following pictures of tick bites may help. Take a moment to review each one closely and read through the accompanying descriptions to better spot and identify potential tick bites on you or your loved ones.

In this photo, the tick is still attached, having burrowed its head into the skin to feed. The redness around the tick indicates inflammation in the skin.

In this photo, the tick is still attached to the skin and appears larger because it has been feeding longer. This is an example of an engorged tick, so called because it has been gorging on blood.
Other bug bites can sometimes resemble tick bites, and therefore, it isn’t always easy to know whether you or a loved one have been bitten by a tick. The following guidelines can help, but it is always best to consult with your healthcare provider if you suspect a tick bite.
- Tick bites are not fluid-filled, whereas bites from ants and other insects are typically pus-filled.
- Location can sometimes help distinguish tick bites from other insect bites because ticks most commonly bite the back of the neck, scalp, groin, and legs.
- Other bug bites, particularly those from fleas or bed bugs, may be multiple in number. Ticks typically bite once and then burrow their head under the skin.
Can you feel a tick bite?
Tick bites are painless, so it’s likely you won’t immediately know that you’ve been bitten. The tick injects an anesthetic into the skin at its point of entry, which helps it avoid detection so it can continue feeding. Many patients with the tick-borne disease Lyme disease don’t recall having a bug bite of any kind.
Do ticks burrow completely under the skin?
In general, ticks do not burrow completely under the skin. They burrow parts of their heads into the skin as they feed, a process that can last for up to 10 days.
Rashes may (or may not) indicate a tick-borne infection
A bulls-eye rash is often a telltale sign—not only of tick bite but of a potential Lyme disease infection. Other bug bites typically do not produce a rash with this distinctive pattern. A bulls-eye rash only appears about 33% of the time when a person has been infected with Lyme disease. Rashes may also indicate other types of tick-borne diseases, including tick-borne relapsing fever, Rocky Mountain Spotted Fever, Ehrlichiosis or Bartonellosis.
If you see this or any other rash pattern near a site, notify your healthcare provider immediately.


The skin is reddened in the area immediately surrounding the tick bite in this picture. Look closely and you’ll also see another “ring” of redness farther out from the site. This is called a bulls-eye rash – also known technically as erythema migrans (EM) rash – and appears only about 33 percent of the time when a person has been infected with Lyme disease.

In this photo, you see the bull’s-eye rash (EM) but no tick.((Chaaya, G., Jaller-Char, J.J., and Ali, S.K. “Beyond the Bull’s Eye: Recognizing Lyme Disease.” Journal of Family Practice 65, no. 6 (June 2016): 373–9. https://pubmed.ncbi.nlm.nih.gov/27474818/.))
Streaked rashes
Lyme is not the only disease that a tick bite may cause. When identifying tick bites, bear in mind that Bartonellosis tends to appear as a slightly different style of rash. These rashes will present themselves in an unusual ‘streaked’ pattern, similar to striae distensae (stretch marks) one might experience on their skin due to pregnancy or rapid weight gain.
The ‘streaks’ of this rash will usually be red or dark brown in color and do not follow skin planes.

In this photo, you see the rash caused by Bartonella.
How long does a tick bite last?
It depends on several factors, including simple individual differences as well as the presence or absence of infection. A tick bite may cause a small, red skin reaction no bigger than the size of a dime that can last days to weeks. This does not necessarily indicate infection but should be noted as a sign of possible exposure.
However, an erythema migrans rash – which is an early sign of Lyme – will grow in size over several days and can develop and grow within the first several weeks of infection.
What To Do After Identifying a Tick Bite
You’ve successfully identified a tick bite, either by seeing the tick firsthand, or by observing a bull’s-eye or streaked rash in the bite area. What should you do if you’ve been bitten by a tick?
Remove the tick
Of course, the most obvious way to identify a tick bite is to recognize that a tick is partially burrowed into the skin.
If you see a tick still attached to the skin, remove it immediately. There are many ways to remove ticks, but some are more effective than others.
Preserving the tick can help your doctor determine whether it carries a potential disease in the event that you develop any symptoms following the bite. Smashing a tick that is attached to your skin can also release more toxins into your body, which can further expose you to potential infectious diseases. So even though your initial inclination may be to squash a tick that has attached to your skin, try instead to keep it intact.
How to remove a tick quickly and safely
The following steps can help you remove the tick quickly and carefully:
- Grab the tick with pointed tweezers close to the skin where it has burrowed in.
- Do not squeeze the tick—that may cause more pathogen-laced saliva to enter the body.
- Pull upward with steady, even pressure. Do not twist or jerk the tick; this can cause mouth parts to break off and remain in the skin. Tick removal can get tricky if the tick’s body breaks apart during removal. If this happens, try to tweeze out the remainder of the tick body or leave it in place and have a healthcare provider remove it as soon as possible.
- You may hear a pop when the tick is removed.
- Place the tick in a ziplock bag and close it tightly. Keep it in the freezer.
- Clean the skin with alcohol and wash your hands.
- Do NOT use cigarette butts or matches.
- If possible, send the tick in to be tested for disease. This can help determine your exposure to disease and also helps with general tick surveillance. Learn more about getting a tick tested through IGeneX.

Grab the tick with pointed tweezers close to the skin where it has burrowed in.
Watch for symptoms
Careful observation is an important first step after identifying any tick bite. Write down the dates and circumstances of any bites you or a loved one encounter, along with any symptoms that present immediately or over time.
General symptoms of tick-borne diseases
If infected with a tick-borne illness, symptoms generally start to present themselves a few days after the bite. Although the symptoms vary based on the type of tick and the disease it may be carrying, general signs to watch for include the following:
- Mild itching
- Reddened area on the skin
- Very specific type of bulls-eye rash (EM) for Lyme
- Non-EM rash for other tick-related infections
- Fever
Some of the diseases carried by ticks include Borreliosis (Lyme disease and tick-borne relapsing fever—TBRF), Babesiosis, Ehrlichiosis, Bartonellosis, Anaplasmosis, Tularemia, and Rickettsiosis (including Rocky Mountain spotted fever). With certain diseases, symptoms may worsen over time. These may include memory loss, muscle weakness, fatigue, fevers that come and go, and declining cognitive functions.
Talk to your doctor
If you see signs of a potential tick-borne illness, be sure to share this information with your healthcare provider. In many cases, patients and their doctors simply don’t realize that a tick bite from several weeks or months ago is responsible for their illness.

Get tested for tick-borne diseases
Testing for tick-borne diseases early and alerting healthcare providers as quickly as possible to any exposure to ticks may contribute to an earlier diagnosis of tick-borne illnesses.
There are many different types of tests for tick-borne diseases. For Lyme disease, the most common tick-borne illness, the CDC recommends a two-tiered testing protocol using an ELISA followed by a Western blot. However, there is a risk for false positives and false negatives with this approach, primarily because these tests are only looking for a single species of borrelia, B. burgdorferi B31. This can lead many people with Lyme or other tick-borne diseases to be misdiagnosed – or even undiagnosed.
IGeneX uses the more inclusive ImmunoBlot assays to test for more species of borrelia, which improves the sensitivity. The specificity of these new tests is also high, at 100 percent for IgM antibodies and 98 percent for IgG antibodies. That substantially higher accuracy can lead to earlier detection of patients. Learn more about testing with IGeneX today.
Testing for tick borne diseases early and alerting healthcare providers as quickly as possible to any exposure to ticks may contribute to an earlier diagnosis of tick-borne illnesses.