What is Lyme Disease?
Lyme disease, also known as Lyme borreliosis, is not only the most well-known tick-borne illness, but also one of the fastest growing infectious diseases in the United States and Western Europe. However, the overall knowledge of the disease among healthcare professionals and the general population alike is still lacking.
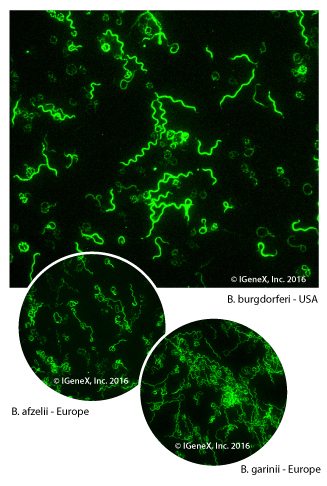
The scientific name of the bacteria that causes Lyme disease is Borrelia. The two most common diseases caused by Borrelia are Lyme disease and Tick-borne Relapsing Fever (TBRF). Both are transmitted via ticks. Borrelia that cause Lyme disease are collectively known as Borrelia burgdorferi sensu lato. B. burgdorferi sensu lato currently includes at least 18 known species of Borrelia. However, new species are continuously being discovered, so the number will probably rise. Three of the most important human pathogenic species of Borrelia are B. burgdorferi sensu stricto in the USA and Europe, and Borrelia afzelii and Borrelia garinii in Europe and Asia.1
How does Lyme Disease get its Name?
In the early 1970s, there was an unexpected outbreak of an arthritis-like condition affecting a group of children and adults living close to Lyme, Connecticut. The group was studied by a medical establishment, and all those infected recalled being bitten by a tick in or around Lyme, Connecticut, leading scientists to name the unknown disease, Lyme.2 The causative agent of Lyme disease was first identified in 1981 by Prof. Wilhelm “Willy” Burgdorfer as a spirochetal bacterium, and was named after him as Borrelia burgdorferi.3 Furthermore, he discovered that the bacteria was spiral in shape and was carried by ticks found on deer. The B. burgdorferi group belongs to the genus, Borrelia, of order Spirochaetales. Lyme disease causing spirochetes are closely related to the spirochete bacterium that causes syphilis.4
How is Lyme Disease Transmitted?
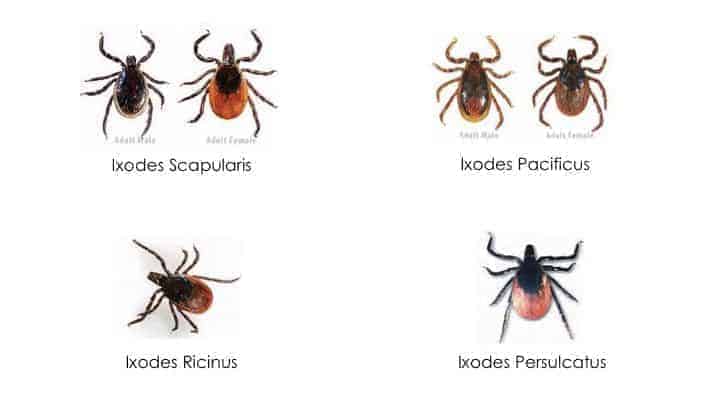
The spirochete Borrelia burgdorferi, a “corkscrew”, spiral shaped bacterium that causes Lyme disease, is transmitted to humans by hard ticks. Currently two species of deer ticks, the eastern black-legged tick, Ixodes scapularis, and the western black-legged tick, I. pacificus, are known vectors for B. burgdorferi, the causative agent of Lyme disease in the US.5 In Europe, Russia, and North Africa the vector is the castor bean tick, I. ricinus, and in Asia the taiga tick, I. persulcatus.6,7
These hard ticks become infected with the bacteria, during the larvae and nymph stages of their lifecycle, while feeding on infected reservoir hosts, such as white-footed mice and birds. The adult ticks are transported by white tailed deer, enabling the dispersion of infected ticks in the wild, and also increasing the proximity of these ticks to larger mammal hosts. Ticks transmit Borrelia to humans by latching on to the host and biting. The tiny ticks feed at a slow pace and may stay on the body for hours to 3 days without the host realizing they are there. The tick engorges itself with blood, and if infected, the spirochete is transmitted to the bloodstream of the person or animal during the bite.8
What are the Symptoms of Lyme Disease?
Over 100 years ago in Europe, before the known causes of Lyme disease were discovered, the illness was first described by the characteristic early stage disease, skin rash erythema chronicum migrans (EM), and by the late stage disease, skin rash acrodermatitis chronica atrophicans (ACA). We now know the European species, B. afzelii, was responsible.9
The symptoms of Lyme disease are similar to those of TBRF, which include fever, headache, fatigue, chills, myalgia, joint and muscle pain, loss of appetite, nausea, disorientation or memory loss, lack of coordination, as well as more severe conditions of neurological disease. Additionally, a characteristic red bulls-eye rash, known as erythema chronicum migrans (EM), may appear at the site of the bite within days to weeks after exposure, but it is present in less than 40% of patients. Nervous system abnormalities may include memory loss and partial facial paralysis (Bell’s palsy). Migratory joint pains, pain in the tendons, muscles and bones may occur later in the disease. Arthritic symptoms, if present, usually affect the large joints like the knees. Symptoms may appear, disappear, and reappear at various times.
Lyme borreliosis caused by B. burgdorferi sensu stricto causes a multisystemic disease that can affect many organs, including the heart, joints, central nervous system, and the brain. B. afzelii causes a distinct skin infection known as ACA, and B. garinii is associated with early Lyme neuroborreliosis, causing painful radiculitis (Garin-Bujadoux-Bannwarth syndrome).10, 11
What is the Geographical Distribution of Lyme Disease?
According to the Centers for Disease Control and Prevention (CDC), around 300,000 people are diagnosed with Lyme disease annually in the US. This does not, however, take into account the number of people that go undiagnosed or are misdiagnosed with other illnesses.12 Lyme disease is not only prevalent in the US, but Europe, the Middle East, and parts of Asia and Australia as well.
Lyme disease is caused by various species of Borrelia with a worldwide geographic distribution:
| Geographical Distribution | Borrelia Species |
| North America | B. burgdorferi sensu stricto (including B31 and B. burgdorferi 297), B. bissettii, B. californensis, B. spielmanii, B. andersonii, B. carolensis, B. mayoni |
| Europe | B. afzelii, B. bavaiensis, B. bissettii, B. garinii, B. kurtenbachii, B. burgdorferi sensu stricto, B. spielmanii, B. lusitaniae, B. valaisiania |
| Asia | B. afzelii, B. garinii, B. lusitaniae, B. valaisiania, B. sinica, B. japonica |
| Australia | B. queenslandica |
How Widespread is Lyme Disease in the United States?
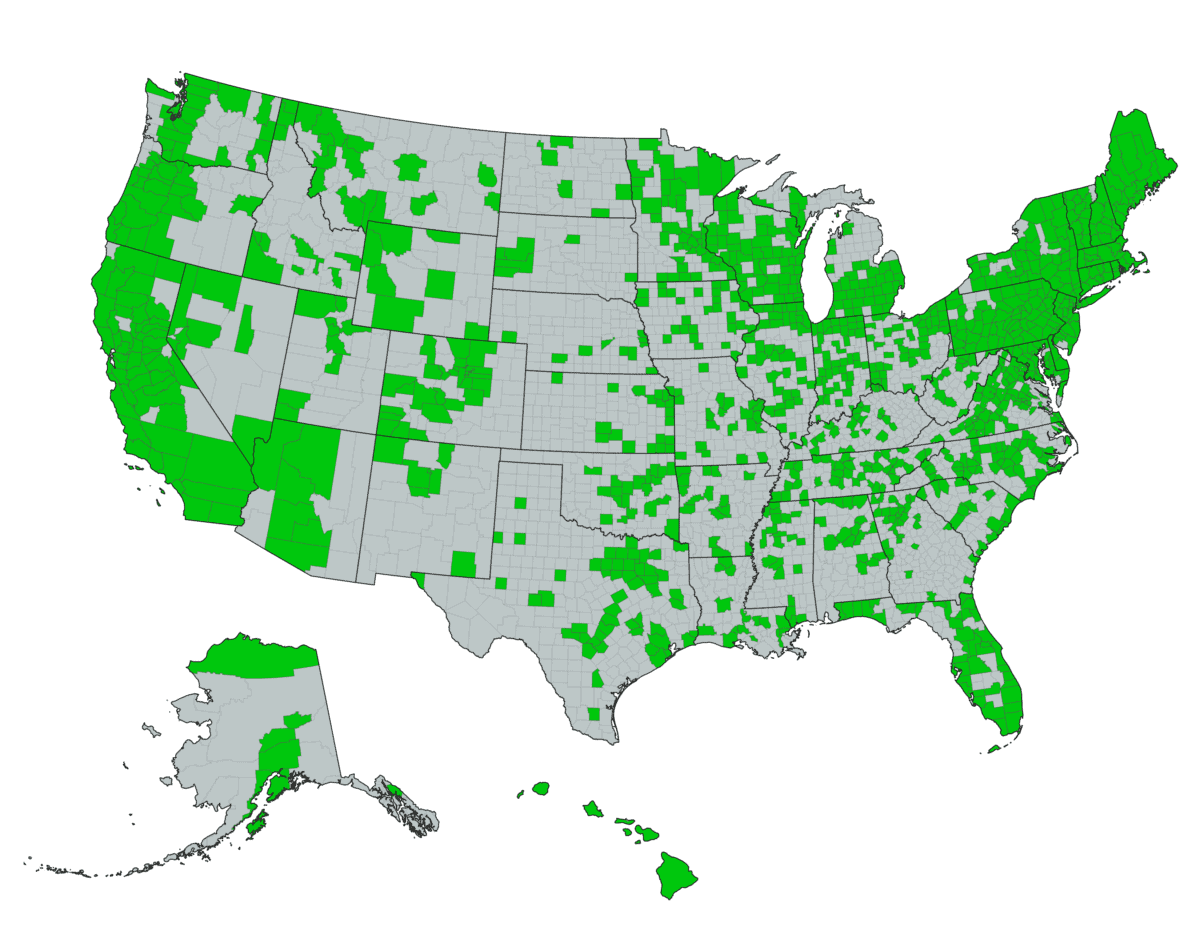
IGeneX Laboratory has discovered Lyme disease in all 50 states, across 1155 counties. Lyme disease was once very concentrated in the Northeast and Upper Midwest, but over the past twenty years has spread to all parts of the United States. The map below illustrates the counties where patients have been diagnosed with Lyme disease.
How is Lyme Disease Diagnosed?
Lyme disease is a clinical diagnosis. Unfortunately, patients with Lyme disease are commonly misdiagnosed with other ailments. Similar to Syphilis in the 19th Century, Lyme disease is known as the “Great Imitator”, and can masquerade as ALS, MS, Chronic Fatigue Syndrome, Fibromyalgia, Alzheimer’s, Parkinson’s, Autism, and other illnesses. Fewer than 50% of patients with Lyme disease recall being bitten by a tick, and most patients aren’t tested for Lyme until they display long term health problems.13
Lyme disease can be diagnosed at a hospital laboratory, or though a lab, such as IGeneX, that specializes in tick-borne diseases. The diagnosis of Lyme disease encounters two main problems: misdiagnosis and late diagnosis. Comprehensive laboratory testing (that includes serological tests such as Lyme Immunoblots [IgM and IgG] to detect antibodies to B. burgdorferi; and Lyme PCR to detect B. burgdorferi specific DNA) offers clinicians the best path to diagnosing their patients. The reasons are: (1) patients with poor immune system , or very early in the disease when antibodies to B. burgdorferi are absent, the Western Blot and Immunoblot tests will not yield any answers. However, the PCR tests may detect the Borrelia DNA. (2) Patients with very high titers of antibodies to B. burgdorferi may be negative by a Lyme PCR test. (3) Patients in late-stage Lyme or very early in the disease can be negative by serological tests and direct detection tests such as PCR and antigen detection. In this case T-cell tests such as Lyme IgX Spot test may be useful. For a complete list of test methodologies for Lyme disease, please go here.
What is the Cure for Lyme Disease?
Lyme disease can be treated with antibiotics. Antibiotics commonly used include doxycycline, amoxicillin, or cefuroxime axetil. Some people may require intravenous treatment with antibiotics such as ceftriaxone or penicillin. Patients should be examined by their healthcare professional before starting any treatment program. The healthcare professional will use clinical symptoms along with laboratory tests to find out whether a patient has Lyme disease or perhaps some other tick-borne infection.
References
1 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3167092/
2 https://www.bayarealyme.org/about-lyme/history-lyme-disease/
3 https://irp.nih.gov/blog/post/2015/02/the-great-willy-burgdorfer-1925-2014
4 https://www.ncbi.nlm.nih.gov/books/NBK2314/
5 https://www.cdc.gov/lyme/transmission/index.html
6 https://www.ecdc.europa.eu/en/disease-vectors/facts/tick-factsheets/ixodes-ricinus
7 https://www.ifsmed.com/conditions-treatments/lyme-disease-diagnosis-and-treatment/
8 https://sphweb.bumc.bu.edu/otlt/MPH-Modules/PH/LymeDisease/LymeDisease4.html
9 https://www.lymeneteurope.org/forum/viewtopic.php?t=491
10 https://wwwnc.cdc.gov/eid/article/22/5/15-1806_article
11 http://www.ajnr.org/content/30/6/1079
12 https://www.lymedisease.org/lyme-basics/lyme-disease/about-lyme/
13 https://www.ilads.org/research-literature/lyme-101-series-at-iladef/