What is Bartonellosis?
Bartonellosis is a group of diseases caused by species of the genus Bartonella and is primarily associated with fleas and lice. However, studies have found that certain Bartonella species are carried by the same ticks that carry Lyme disease, and ticks are likely the chief source of human Bartonellosis infection. Therefore, Bartonellosis can be seen as an emerging tick-borne infection.
Several species of Bartonella cause severe diseases in humans, such as Cat scratch disease (CSD), endocarditis, trench fever, and Carrion’s disease. Currently, around half the species of the gram-negative bacterial genus Bartonella are known to cause human disease. Some of these species include B. elizabethae, B. washoensis, B. vinsonii, B. koehlare, and B. alsatica
Cat Scratch Disease
Bartonella henselae is the causative agent for CSD and has also been known to cause bacillary angiomatosis, peliosis hepatis, bacteremia, and endocarditis in immunocompromised individuals.[1]
CSD was first described in 1931, but the causative agent was unknown at the time, so CSD was not reported until decades later, in 1990.
Trench Fever
Bartonella quintana causes trench fever, described as such due to outbreaks during WWI and WWII. Fewer cases were reported after the wars, but during the 1990s, infections caused by B. quintana were re-emerging among destitute populations in the US and Europe.
Carrion’s Disease
Carrion’s disease is caused by B. bacilliformis, and is only known to infect humans. The first reported outbreak occurred in 1871, causing over 4,000 casualties.[2].[3]
How is Bartonellosis transmitted?
Bartonellosis can be transmitted through a number of avenues, depending on the Bartonella species.
Cat scratch disease is most often transmitted to humans from a bite or scratch of an infected cat. Cats contract B. henselae from the bite or droppings of cat fleas. Cat fleas are thought to amplify the B. henselae reservoir and not directly transmit the disease to humans.
In recent years it has been believed that B. henselae may also be a tick-borne pathogen and can be present in the same Ixodes ticks that transmit pathogens causing Lyme disease, Tick-Borne Relapsing Fever, Babesiosis, and Ehrlichiosis.[4]
Carrion’s disease, caused by B. bacilliformis, is transmitted to humans through the bite of the female sand fly, Lutzomyia verrucarum.
Phases of Bartonellosis
The disease presents in two distinct phases, with the bacteria invading the erythrocytes during the acute phase and the endothelial cells during the chronic phase.[6] Recently, scientists have determined the transmission of Bartonella to mice via ticks.
Animals that can harbor Bartonella infected ticks
The animals listed in the table below can harbor infected fleas or ticks that carry Bartonella. The disease occurs most frequently in children under 15 years.
| Species of Bartonella | Reservoir | Vector |
| B. henselae | Cat | Flea and Tick |
| B. quintana | Human/ cat | Louse |
| B. elizabethae | Rat | Flea |
| B. washoensis | Ground squirrel | Flea |
| B. vinsonii arup | Mice | Tick |
| B. vinsonii berk | Cat | Tick |
| B. koehlare | Cat | Flea |
| B. alsatica | Rabbit | Scratch |
| B. bacilliformis | Human | Sand Flies |
What are the symptoms of Bartonellosis?
The symptoms of Bartonellosis can vary from mild to severe, and usually begin 5 to 14 days after infection. Common symptoms of Bartonellosis include:
- Fever
- Headaches
- Fatigue,
- Poor appetite
- Brain fog
- Muscle pain
- Swollen glands around the head, neck, and arms
Bartonella rashes
Part of identifying tick bites is knowing the difference between the rashes associated with infected bites. While Lyme disease can sometimes present itself as erythema migrans, or a bull’s eye rash, a Bartonella rash is not quite the same.
If a Bartonella rash appears, it will be in a ‘streaked’ pattern, similar to stretch marks. To tell the difference, know that a Bartonella rash will not go with the plane of the skin as stretch marks do.
Symptoms of CSD
Symptoms specific to CSD comprise enlarged lymph nodes, a papule or pustule at the inoculation site, and, on rare occasions, complications affecting the brain, eye disorders, severe muscle pain, hepatosplenic infection, osteomyelitis, and encephalitis.
These rare manifestations are more common in children younger than five years due to their weakened immune systems. Infection by B. quintana, the causative agent of Trench fever, specifically includes symptoms of skin rashes, recurrent fevers, and rarely, heart failure. In immunocompromised patients such as those with HIV, the potentially fatal disease bacillary angiomatosis, caused by B. henselae or B. quintana, can occur.
Symptoms of Carrion’s disease
The symptoms of Carrion’s disease, caused by B. bacilliformis, present in two distinct phases: Oroya fever and Verruga peruana (Peruvian warts). Oroya fever is very similar to malaria, characterized by high fever, sweating, headaches, chills, and weakness. Whereas, Verruga peruana develops in the second stage of Carrion’s disease and is characterized by reddish, purple skin lesions.
Other symptoms of Bartonellosis
Some other symptoms of Bartonellosis include photophobia, tachycardia, bowel problems, OCD behavior, anxiety, rapid relapse off of antibiotics, psychiatric problems, pain behind the eyes, and no response to previous antibiotic treatments.[7] [8]
Long-Term Bartonella Symptoms
As with Lyme disease, there is the possibility of long-term Bartonella symptoms, as noted in some cases. These include low-grade relapsing fever and chronic eye problems, such as blurred vision or irritation.
Other long-term Bartonella symptoms that some have reported include soreness in the soles of the feet in the morning, likely caused by trauma to the blood vessels there.
Some have also indicated anemia among their long-term Bartonella symptoms, as well as neurological symptoms like decreased cognition, memory impairment, insomnia, and restlessness.
Long-Term Bartonella Symptoms
There is the possibility of long-term Bartonella symptoms, as noted in some cases. These include low-grade relapsing fever and chronic eye problems, such as blurred vision or irritation. Other long-term Bartonella symptoms that some have reported include soreness in the soles of the feet in the morning, likely caused by trauma to the blood vessels there.
Some have also indicated anemia among their long-term Bartonella symptoms, as well as neurological symptoms like decreased cognition, memory impairment, insomnia, and restlessness.
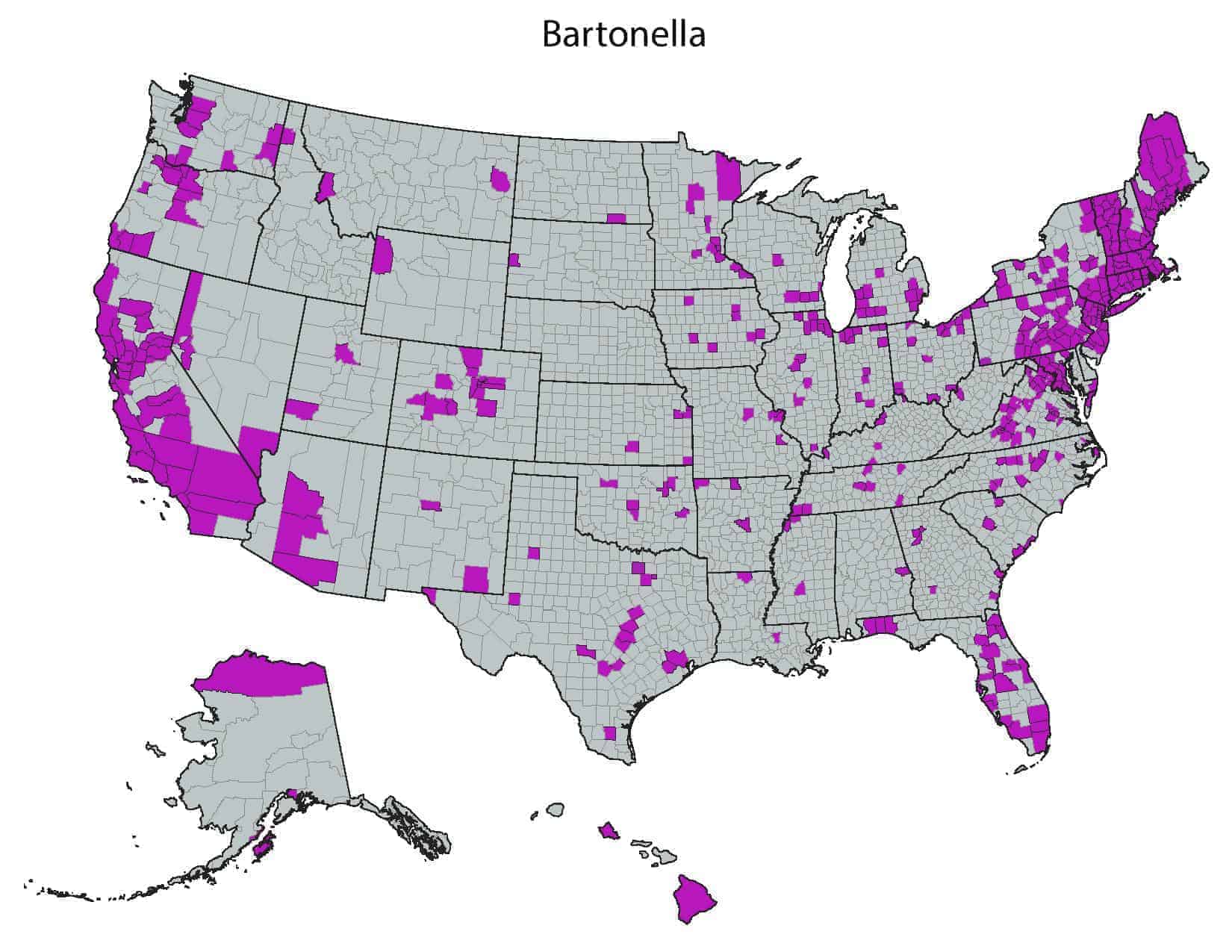
What is the Geographical Distribution of Bartonellosis?
Bartonellosis is found worldwide. In a study of Ixodes pacificus, Western blacklegged ticks collected in California, 19.2% were found to be carrying Bartonella. Five different species of Bartonella were detected.[9] CSD occurs worldwide and may be present wherever cats, ground squirrels, mice, and rabbits are found.
Trench fever also has a worldwide distribution and is commonly associated with homeless populations, overcrowding, and areas of poor sanitation.
Carrion’s disease, previously thought to be endemic to Peruvian Andes, has been found in other South American countries too, especially in high altitude valleys[10]
Bartonella has been found in 49 out of 50 US states.
How is Bartonellosis Diagnosed?
How is Bartonellosis Diagnosed?
The diagnosis of Bartonellosis should be considered in patients bitten by a tick or flea, or scratched by small animals and who are experiencing any of the symptoms typical of Bartonella infections, even mild ones. Cases of CSD can usually be diagnosed via the patient’s symptoms and history.
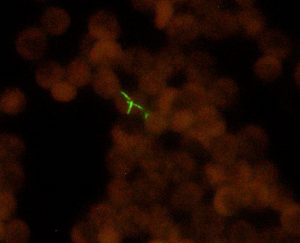
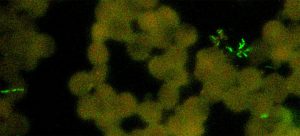
However, laboratory tests such as IFA (Indirect Immunoflurescent Assay), Western Blots, PCR (Polymerase Chain Reaction), and FISH (Fluorescent In-Situ Hybridization) tests are important to confirm the diagnosis and verify the possibility of cross-reaction with any other species of Bartonella that can be transmitted by ticks.[11] When testing for B. henselae, testing for other tick-borne illnesses should also be considered.
Patients should be examined by their healthcare professional. The healthcare professional will use clinical symptoms along with laboratory tests to find out whether a patient has Bartonellosis or perhaps some other tick-borne infection. Consult your doctor about ordering an IGeneX testing kit to detect Bartonellosis.
[1] https://pubmed.ncbi.nlm.nih.gov/15298152/
[2] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4102455/
[3] https://www.columbia-lyme.org/bartonellosis
[4] https://www.cuimc.columbia.edu/
[5] https://ecdc.europa.eu/en/bartonella-quintana-infection-trench-fever/facts
[6] http://www.benbrew.com/lb/bartonella8.pdf
[7] https://www.cdc.gov/bartonella/symptoms/index.html
[8] https://www.columbia-lyme.org/bartonellosis
[9] https://www.lymedisease.org/lyme-basics/co-infections/bartonella/
[10] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4102455/
[11] https://www.columbia-lyme.org/bartonellosis