Every year, about 400,000 people in the United States are diagnosed with Lyme borreliosis, commonly known as Lyme disease, based on Centers for Disease Control and Prevention (CDC) estimates of reporting. This does not include cases of Tick-Borne Relapsing Fever (TBRF), which is caused by another group of Borrelia but has similar symptoms to those of Lyme disease.
That’s more than the number of people diagnosed annually with either breast cancer or HIV/AIDS in this country. Yet despite its prevalence, Lyme disease is an illness that most people know relatively little about.
The following article can shed light on key aspects of the disease, including how it is transmitted, how to reduce the risk of infection, what symptoms to watch for, the most accurate tests for Lyme disease, and how Lyme disease can be treated. Whether you’re concerned that you or a loved one may have contracted Lyme disease or you’re just interested in learning more about it, these facts and resources can address some basic questions while deepening your overall understanding of this complex and often-misdiagnosed disease.
Lyme Disease Basics
1. Lyme disease is a tick-borne bacterial infection.
Lyme disease is an infectious disease caused by several species of spiral-shaped bacteria from the group Borrelia. Certain species of ticks can transmit the disease to humans and animals when they bite into the skin to feed. In the United States, the black-legged tick (Ixodes scapularis) – also known as the deer tick – and the related Western black-legged tick (Ixodes pacificus) are the primary carriers of Lyme disease.
Although ticks of any size or age can transmit Lyme disease, most people are infected by immature ticks, called nymphs, which are very small (only about 2mm in size) and therefore less likely to be discovered and quickly removed.
That’s important because the longer an infected tick is attached to the skin, the higher the chances are of transmitting the disease. The CDC states that in most cases, an infected tick must be attached for 36 to 48 hours or more before the Lyme disease bacterium can be transmitted.
2. Lyme disease can affect anyone, almost anywhere.
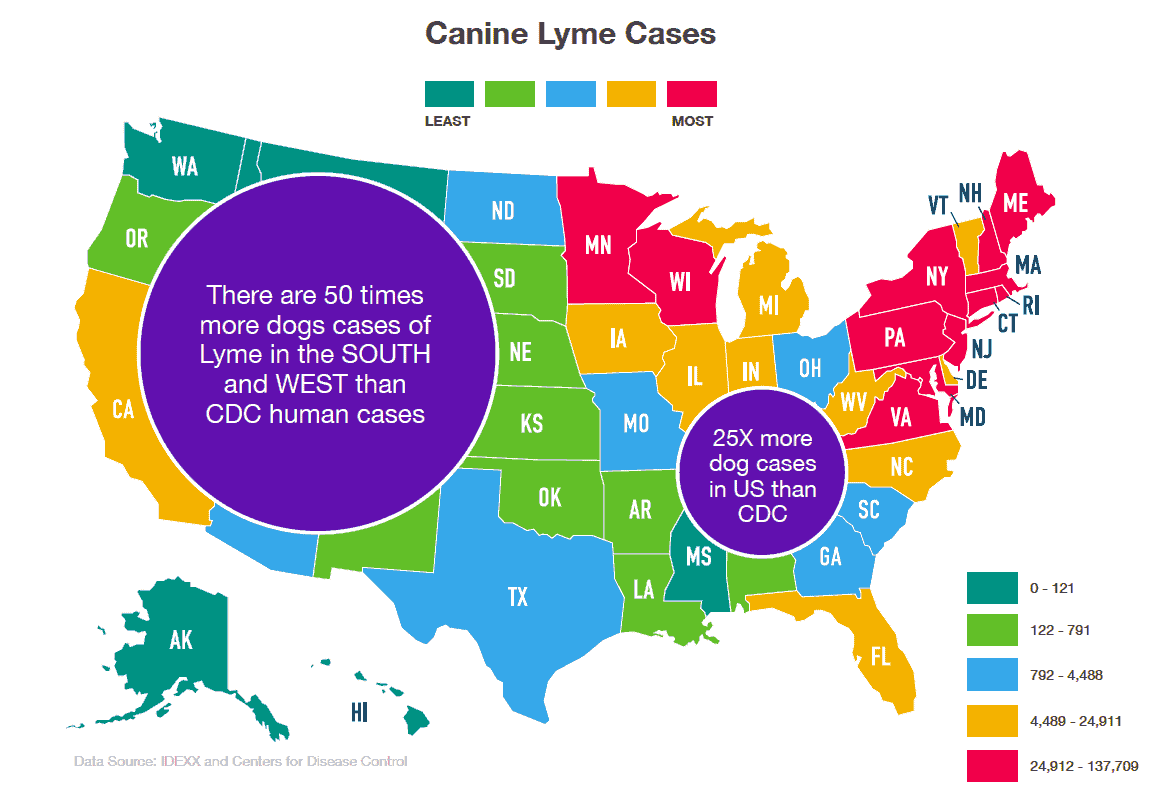
Lyme disease occurs in all 50 states, as well as more than 60 countries around the world. The disease can affect people of all ages, as well as animals—including dogs, cats, and horses. Within the United States, certain regions have higher rates of infection than others.
Risk maps from the CDC, IGeneX and other sources can help you identify areas with the highest number of human Lyme disease cases.
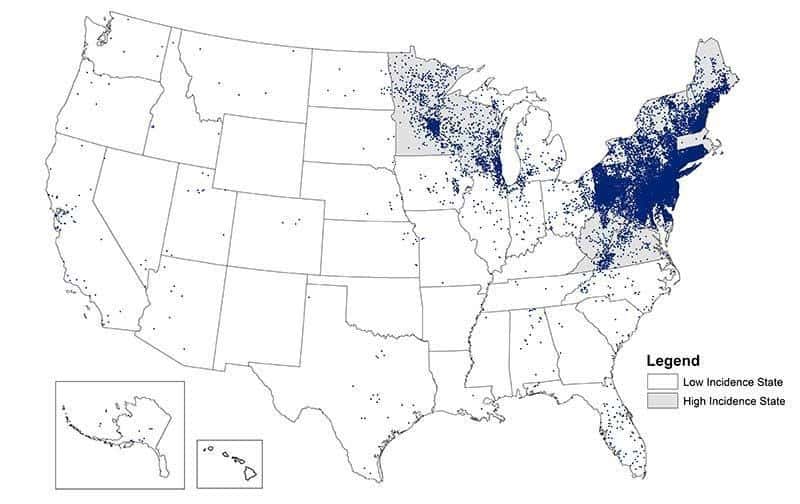
Reported Cases of Lyme Disease — United States, 2018 (Source: CDC)
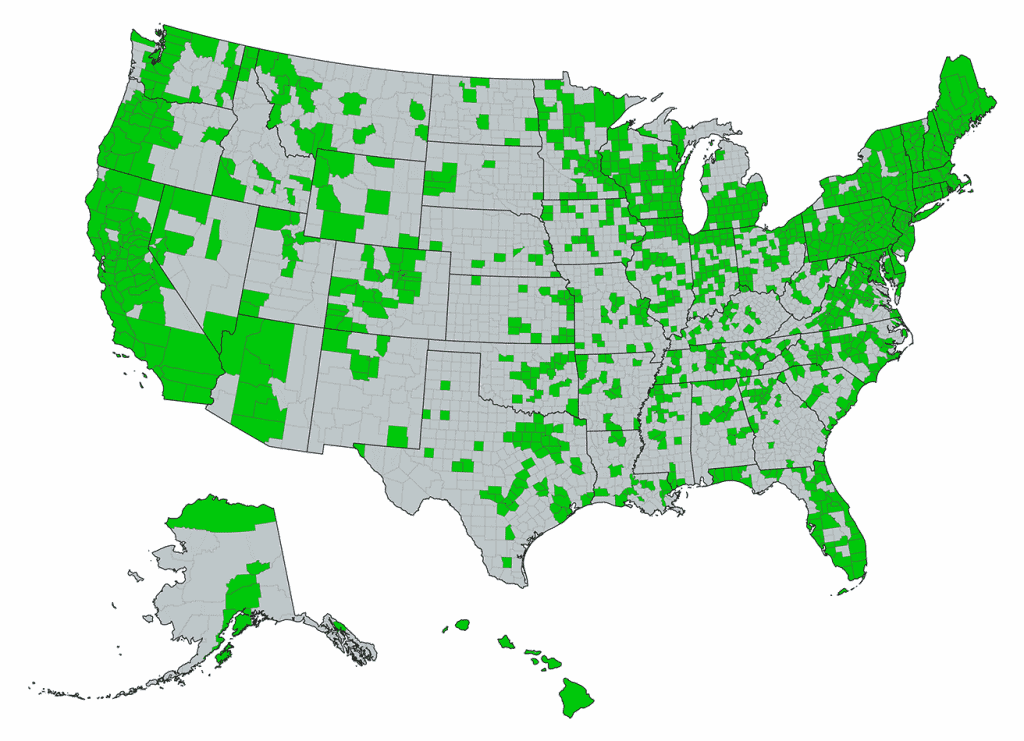
Counties with at least one incidence of Lyme disease in 2019 (Source: IGeneX)
Keep in mind, however, that most risk maps only reflect the total number of reported cases in an area, which, due to misdiagnoses or other factors, may be less than the actual number of people infected. According to lymedisease.org, the best maps of risk actually may be canine maps, because dogs are regularly screened for Lyme disease through a nationwide program.
3. Preventive steps can help lower risk.
In general, tick populations tend to be higher in wooded and grassy areas, where the animals they feed on live and roam. When you are in these types of environments, a few simple precautions may help lower your risk for getting Lyme disease.
For example, wear close-knit clothing, and check your skin, clothes, and shoes frequently for ticks. Try to avoid contact with soil, vegetation, and leaf piles around trees, and stay on wide, open trails as much as possible. Wear a hat, tie back long hair, and make sure to do a final scan for ticks at the end of the day—especially on children and pets. You can find additional prevention tips and suggestions in the accompanying list of resources, or check out IGeneX’s guide to preventing tick-borne disease.
4. Lyme disease can be difficult to detect and diagnose.
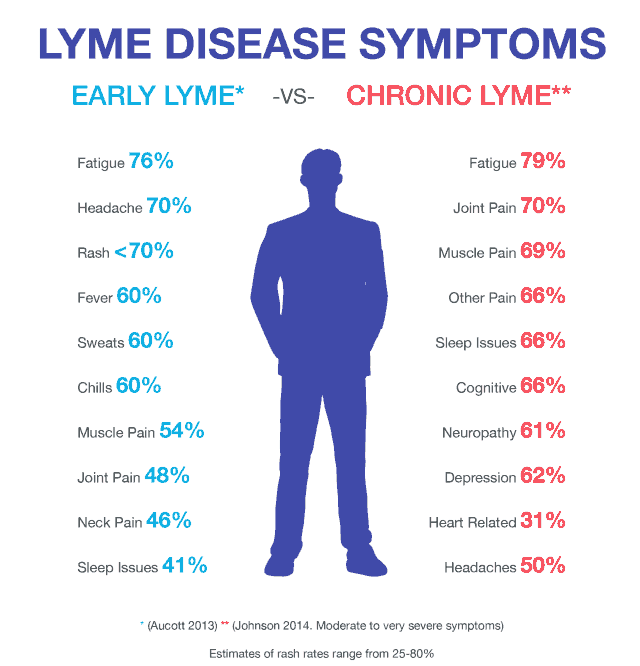
If you have been infected with Lyme disease, symptoms may appear anywhere from three days to a month after being bitten. Early on, symptoms may be flu-like, including fever, chills, headache, fatigue, swollen lymph nodes, and achy joints and muscles. Some people also develop a rash at the site of the bite or elsewhere on their body.

A bulls-eye-shaped rash is one of the most recognizable signs of Lyme disease, but not everyone develops a rash or one that follows this distinctive pattern. In fact, fewer than 50 percent of people diagnosed with Lyme disease recall having any kind of rash.
If Lyme disease isn’t diagnosed and treated early on, it can develop into late-stage or chronic Lyme disease. As the infection has more time to spread to different systems and areas of the body, patients with chronic Lyme disease may experience a wider range of symptoms that are more severe. These can include headache, fatigue, joint pain and swelling, cognitive difficulty, facial drooping (Bell’s palsy), depression, sleep disturbances, heart palpitations or shooting pain, or numbness or tingling in the hands or feet.
Lyme disease is often called “the great imitator,” because its symptoms closely resemble other conditions and illnesses, including:
- Chronic Fatigue Syndrome
- Fibromyalgia
- Rheumatoid Arthritis
- Multiple Sclerosis
- Parkinson’s Disease
- ALS
- Depression
- Alzheimer’s Disease
Alerting your healthcare provider to any exposure you might have had to areas and environments at risk for Lyme disease could help lessen the chance of misdiagnosis. Certain laboratory blood tests can help confirm a diagnosis when Lyme disease is suspected.
5. Antibiotics are the only known effective treatment for Lyme disease.
When diagnosed and treated with appropriate antibiotics in the early stages of Lyme disease, patients often recover quickly and completely. Patients who are treated in the later stages of the disease tend to require longer-term antibiotics, including intravenous antibiotics. They also may incur long-term damage to their joints or nervous system.
Following treatment, many patients may continue to experience some symptoms of the disease for a period of time. In some cases, symptoms can last for six months or longer. The International Lyme and Associated Disease Society (ILADS) states that without proper treatment, people with chronic Lyme disease may experience ongoing symptoms—such as severe fatigue, anxiety, headaches, and joint pain—resulting in a poorer quality of life than patients with diabetes or a heart condition.
As with any illness, early detection and treatment of Lyme disease is important. If you suspect that you or a loved one may have contracted it, consult with your healthcare provider as soon as possible.
Testing, Treatment, and Diagnosis
Getting tested for Lyme disease
Lyme disease is often misdiagnosed or entirely missed at early stages. As mentioned above, this can allow the disease to develop into more severe and/or chronic Lyme disease down the road. This is why it’s so important to get an accurate diagnosis as early as possible.
There are a few factors that influence a person’s ability to get a reliable diagnosis. One is the timing of the test. Because even the most accurate Lyme disease tests detect antibodies, not the pathogens themselves, it’s important not to get tested too early after possible exposure. If you test too early with conventional tests, you may not have enough antibodies yet, and the test results could be negative even though you do have an infection. However, there are tests that specialize in early detection – IGeneX offers one, the IgXSpot test.
It’s also important to recognize that there are at least 18 distinct types of Borrelia that cause Lyme disease, and if your test is only designed to detect one or two types – which is unfortunately all too common – it will miss infections caused by other types. The most accurate tests for Lyme disease are designed to detect all the different types of Lyme disease bacteria found in North America and Europe.
To learn more about what makes certain types of Lyme disease tests more reliable than others, read IGeneX’s blog on the most accurate test for Lyme disease.
Can a tick be tested for disease?
Yes, a tick can be tested for Lyme disease. In fact, if you find a tick on you, you can and should send it to IGeneX for testing.
Distinguishing between Lyme disease and Tick-Borne Relapsing Fever
Tick-borne relapsing fever (TBRF) has some similarities to Lyme disease, but they are in fact very distinct diseases that require specific treatment and monitoring by healthcare professionals.
One of the biggest points of similarity between the two diseases is the fact that they are both caused by Borrelia bacteria. However, the genus Borrelia divides into two very distinct groups: Borrelia burgdorferi, one of the primary types of Lyme disease bacteria, and relapsing fever Borrelia, which causes TBRF.
These bacteria are further distinguished by the fact that they are transmitted by different types of ticks. As noted earlier, Borrelia burgdorferi is transmitted by either the black-legged tick (Ixodes scapularis) or the related Western black-legged tick (Ixodes pacificus), both of which are part of the “hard tick” family. Hard ticks all share the distinguishing trait of a hard outer shield or back plate, known as a scutum.
By contrast, relapsing fever Borrelia is transmitted by certain species of “soft ticks”—a different family of ticks that do not have a scutum but instead have more rounded bodies. Soft ticks also prefer a different habitat than hard ticks and feed very quickly, often attaching and falling off hosts in less than an hour. However, recently B. miyamotoi, which falls in the TBRF group, has been found in Lyme endemic areas being transmitted by hard ticks, the same ticks that transmit Lyme.
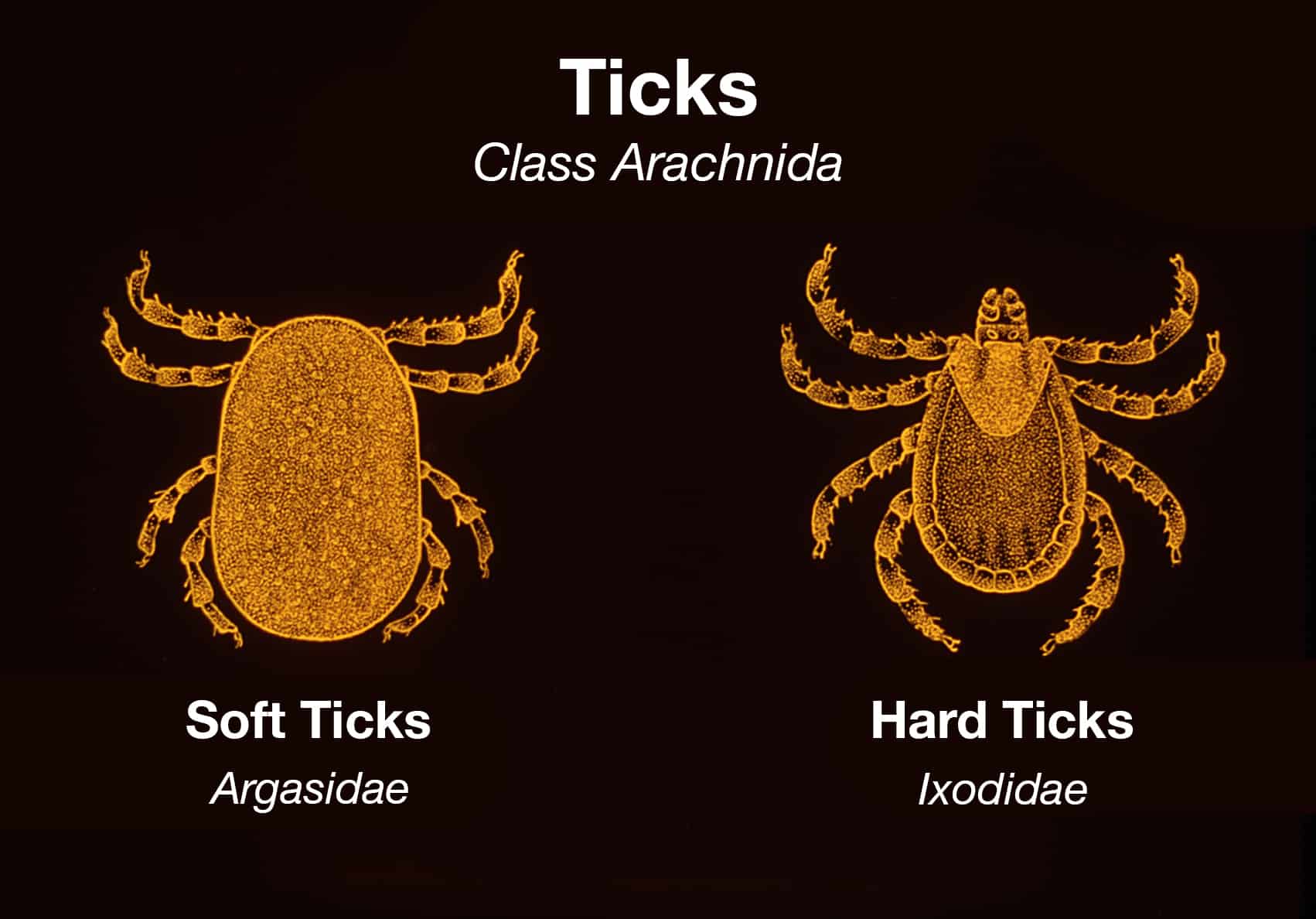
Image Source:https://phil.cdc.gov/Details.aspx?pid=5993
Hard ticks all share the distinguishing trait of a hard outer shield or black plate, known as a scutum.
SOFT TICKS (ARGASIDAE)
Soft ticks do not have a scutum but instead have more rounded bodies.
Both Lyme disease and TBRF have similar initial flu-like symptoms. However, TBRF symptoms typically present, resolve, and relapse continuously over specific time frames. And although both diseases can be treated effectively with antibiotics, they require different types of drugs and treatment courses to resolve the respective infections.
If you suspect that you or a loved one may have contracted either disease, consult with your healthcare provider immediately to accurately diagnose Lyme disease and other tick-borne diseases and treat the illness.
Additional Resources
- https://www.lymedisease.org/lyme-basics/lyme-disease/symptoms/
- https://www.ilads.org/research-literature/lyme-101-series-at-iladef/
- https://www.cdc.gov/lyme/index.html
- https://www.cdc.gov/lyme/resources/brochure/lymediseasebrochure.pdf
- https://www.webmd.com/rheumatoid-arthritis/arthritis-lyme-disease?page=2#3
- https://www.aldf.com/
- https://www.niaid.nih.gov/diseases-conditions/lyme-disease
- https://www.pethealthnetwork.com/dog-health/dog-diseases-conditions-a-z/dogs-ticks-and-tick-borne-parasites/
- https://www.cdc.gov/ticks/diseases/trends.html
- https://www.cdc.gov/relapsing-fever/resources/15_260166_FS_APerea.pdf
- https://www.cdc.gov/relapsing-fever/transmission/index.html